Using Telehealth Technology in Response to COVID-19
Allie Clark | 10 min read | March 6, 2020
[Updated on November 20, 2020]
Our world is in the throes of what is undeniably one of the most severe infectious disease outbreaks in modern history. Coming up with innovative approaches to stem the spread of the infection of this full-blown pandemic is imperative, especially rates of infection once again pick up speed. Global efforts to manage the epidemic quickly and effectively have been overwhelmingly focused on telemedicine technology. Remote care modalities, like in-home video visits, have assisted in both tracking and reducing spread.
The following details provide an update on COVID-19 response locally and around the world, and telemedicine’s role in that response; including policy changes that encourage more U.S. Healthcare facilities to use in-home video visits to help the cause.
Current Status of COVID-19
What is it?
COVID-19 is a disease caused by the novel (new) coronavirus SARS-CoV-2. The main symptoms are fever, cough, and difficulty breathing, but can increase in severity to include pneumonia, multiple organ failure, and even death.
How many cases?
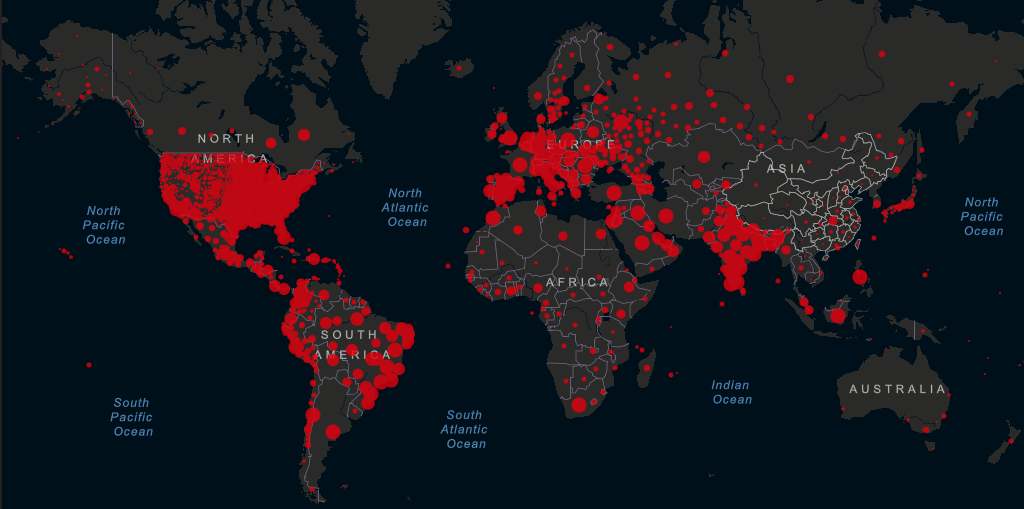
Currently there have been 57,905,684 cases cumulatively. The United States has had 12,274,726 cases to date. For updated World Health Organization situation reports, go here; for United States updates from the Centers for Disease Control, go here.
How many recovered? How many deaths?
40,105,102 people have recovered from the virus; 1,377,584 have died. There have been 260,283 deaths in the US. The worldwide average death rate is now figured at 2.3% – for comparison purposes, the death rate for influenza in the 2018-2019 season was less than 0.1%. This does not take into account the unknown outcomes of currently active cases (of which there are 16,422,998,) unreported cases (which could be as much as 10 times the number of confirmed cases,) or actual deaths (as much as twice the number of confirmed deaths.) As another comparison, in the middle of the SARS epidemic in 2013, the World Health Organization reported a death rate of 4%; the final calculations after the epidemic ended tallied it at 9.6%.
How many countries? How many US states?
The virus is active in 218 countries or territories and 2 international conveyances. In the US, 50 states and Washington D.C. have confirmed or presumptive positive cases.
These numbers change by the hour. For a comprehensive, updated view of current cases and their locations, deaths, and recovered cases, check out this interactive live dashboard from researchers at Johns Hopkins University. Our new favorite updated information site, including some great data visualization aides, is this one from Worldometers.
In the U.S., we have had the ability to test at a large enough scale to handle the speed of viral spread we have been seeing for some time, even after some snafus with the first round of CDC testing kits and guidelines that were so strict they were likely to have missed early incidents of community spread cases. The virus is on the rise again as we write – the current spike we are in started in early October. We are now seeing daily new cases at two and a half times the highest rate in the second spike in mid-July. There is still no vaccine; much of the information in the CDC guidelines and recommendations is based on the behavior of other viruses in the same genetic family as this one. We are getting better at treating it: currently, we are still sitting below the average daily death rate of 2,500 we saw in mid-April. The rate is rising however, with the 3 day average jumping by over 1,000 in the last three days alone. We are growing to understand this virus, though it is slow going. We know the estimated incubation period is 2-14 days, but we have outliers of anywhere from 19 to 20 days. We know if can spread on surfaces, most often in the air in droplets or through person-to-person contact, and possibly by animals. We know it can live outside of a human host for anywhere from 3 hours to 72 hours, depending on the surface and environment. Much of this information is very recent, and has changed drastically since the emergence of this virus on a global scale earlier this year. Experts say that herd immunity is what it will take to truly end this pandemic. However, even with a vaccine in the works, herd immunity is a far-off reality, if a reality at all.
Globally, the response was swift, but so was the virus. The countries most affected in the early days were China, where the virus originated, then the Republic of Korea, Italy, and finally Iran. Currently, the United States takes the prize, with India coming in at about 9 million total cases, and Brazil following at 6 million. The spread of the disease in many early- and highly-affected countries was slowed by lock-downs, hygiene measures (like hand washing and face masks,) and social isolation, but has continued to be supported mainly by virtual healthcare delivery more than any other single strategy. Notably, the slowing of the explosive spread of the virus as it began in China can almost be entirely attributed to telemedicine and virtual care – millions of Chinese citizens are turning to telemedicine for everything from a cough to mental health, as reported by Reuters. This approach was applied to those with symptoms, but even more so to those who are infection free, as a way to encourage them to stay home even when there were medical concerns that would normally necessitate a trip outside. Israel, famous for its robust national health system with a full, government-funded national telehealth network, used this modality exclusively to monitor and communicate with the 12 quarantined passengers who returned home from the Diamond Princess quarantined cruise ship, without exposing a single healthcare worker to the virus. Ontario, Canada, which also boasts a province-wide, government-sponsored telehealth network called Telehealth Ontario, successfully used its free advice line to triage infected individuals at the airport, as reported by The Washington Post.
How telemedicine has aided the effort
Seeing the potential and global success of using virtual healthcare technology to stem or at least slow the tide of this outbreak, experts in America called on healthcare systems, insurance payers, and legislators to expand access to telemedicine technology so that we can do the same. Our country’s healthcare stakeholders responded with a swath of interim rules, legilsation, allowances and agreements. To see a full list of public health emergency-related legislation, see the Center for Connected Health Policy’s summary of federal legislative efforts and state legislation.
Early on, the CDC released a set of recommendations entitled: “Interim Guidance for Healthcare Facilities: Preparing for Community Transmission of COVID-19 in the United States.” Their number one recommendation for “all U.S. healthcare facilities”? Integrate and utilize telehealth. In the document they state: “Shifting practices to triaging and assessing ill patients (including those affected by COVID-19 and patients with other conditions) remotely using nurse advice lines, provider “visits” by telephone, text monitoring system, video conference, or other telehealth and telemedicine methods can reduce exposure of ill persons with staff and minimize surge on facilities.” They highlight various ways the technology can be used and ways to “promote increased use of telehealth” and “explore alternatives to face-to-face triage and visits,” in preparation for the eventual epidemic.
While there are advances made to technology on a daily basis when it comes to virtual care, with the COVID-19 crisis the ability to connect with your patient remotely has permanently changed from “this would be cool” to “we need this now.”
Five (More) Reasons to Use Telehealth During the COVID-19 Outbreak
1. Protect healthcare staff
During the Ebola outbreak of 2014, the healthcare workforce was the first to be infected in large numbers and, according to a technology consultant on the ground in Africa at that time, this was due to a lack of preparedness, especially in the form of use of telehealth technology. The less we can expose our healthcare providers to this virus, the better – we are going to need everyone we have in the coming months more than ever before.
2. Protect the uninfected
As seen in China, perhaps the greatest use of telemedicine in this epidemic is to keep people at home, or at least away from hotbeds of infection transmission such as health clinics, hospitals, and doctor’s offices. It can help in management of chronic disease, which is one of the biggest factors in cases where COVID-19 has led to serious disease and death.
3. Protect mildly ill from complications
Similarly, for those who are already infected, telemedicine can be used to increase the chance that their symptoms stay mild. About 80% of the cases only show mild cold-like symptoms; 56% of patients diagnosed have since recovered. Keeping those patients whose immune systems have been compromised by this virus safe from secondary infections and complications is paramount to stopping the mortality rate from rising any more than it already has.
4. Increase access to care
At the end of 2019, there were 7,655 Primary Medical Health Professional Shortage Areas in the US. Those areas of the country are at a higher risk of community spread of this infection as they are less likely to seek care because of the increased effort it takes to reach a care provider. Having telemedicine readily available at as many community hubs as possible, or even in a client’s home, can greatly reduce the risk to this population.
5. Decrease time to care
Early research has shown that the earlier in the progression of the disease that supportive care is given and treatment is received, the more favorable the outcome. With the level of concern as high as it is, wait lists are full, appointments are double-scheduled, and the more access and availability can be expanded, the greater the chance is that we can stop the spread and lower the mortality rate of this epidemic in our own communities.
It is widely recognized that the success in other countries that can be attributed to telehealth will be hard to replicate in the U.S. if regulatory, legislative, and industry standards and restrictions remain as they are currently. Between inconsistent private payer parity laws, a wide spectrum of state Medicaid requirements, and highly restrictive and outdated Medicare regulations, our collective ability to support communities with the power of telehealth has been ham-stringed. It’s not too dramatic to say that unless something changes in the national telehealth landscape, the health of our country as a whole could be in serious trouble.
In response, the House and the Senate have both passed a $8.3 billion supplemental appropriation fund proposal, which includes $500 million specifically designated to support and expand telehealth resources during and around this crisis. The bill also allows the Department of Health and Human Services, in an “emergency area” during and “emergency period”, to waive the originating site requirement and allow Medicare recipients to receive telehealth care in their home and on their phones through audio-video interactions. This bill has been signed into law and the Secretary of HHS in conjunction with CMS have now released the updates to Medicare policy.
To read the updated Fact Sheet about Medicare and all other coverage changes for telehealth during the crisis from the Center for Connected Health Policy, which serves as the National Telehealth Policy Resource Center for the US, start here.
The value of using video visits for remote care realized
Perhaps this crisis has become the moment telehealth proponents have been waiting for. In an excellent article from STAT News, Eric Perakslis, a doctor at Duke University who was a large part of the technologic response efforts to the Ebola outbreak in West Africa, is quoted as calling telehealth technology “a force multiplier that helps protect health workers and extends their reach, and should absolutely be seized upon.” Both the director of the CDC’s National Center for Immunization and Respiratory Diseases and a senior WHO official who led a recent mission to China implied that telehealth would be integral to America’s fight against this epidemic.
Many news outlets, stakeholders, and governmental agencies have put forth ideas as to how telehealth can be best utilized to support our healthcare facilities and providers as we move past this “tip of the iceberg” of this epidemic, as the Hospital Director at EvergreenHealth in Washington called it on Sunday. There is no question that telehealth is a critical part of the answer we are looking for, but we would posit that the question of “how” is just as important as that of “what for.”
Ease-of-use could be the most important concept for those wanting to add telemedicine services during this crisis. COVID-19 has been wreaking havoc on the economy, and it’s not showing signs of letting up any time soon. People are pouring any extra funds into stocking up on daily and medical supplies in the case of a quarantine or a more widespread outbreak that requires a greater degree of social isolation. Medical compliance is paramount to stopping the spread of this virus and making it available to anyone with whatever they already have will be more important than ever, as purchasing new devices or applications will not be high on anyone’s list in the current climate. Make it easy for your patients to receive remote care – in a time full of uncertainty and anxiety, the last thing people need is to deal with learning a new technology or skill. Finding a way to plug your medical services into the electronic world most consumers already use and experience in their daily life could make a world of difference during this outbreak. The less change the better. The status of our very health and safety seems to be changing at an hourly rate; allowing patients to feel secure in their own routines could help with the mental health side effects of this epidemic as well. In terms of medical practices, it is also important to cut down on workflow disruption as much as possible, as it can add to the length of time from initiation of services to delivery services and right now, that process needs to be made as swift as it can be.
In order to make the process of providing virtual care during this crisis as painless as possible, here are some things to consider:
Five Ways to Best Use Telehealth Technology During the COVID-19 Outbreak
1. Use devices people already have
2. Consider taking advantage of platforms or modalities people already use
3. Lowest amount of prep, installation, training, and workflow change possible
4. User-friendly experience for both provider & patient
5. Minimize potential for IT issues with in-person support and easy-to-use tech
COVID-19 is a real crisis we are facing as a global community. It is apparent that the need to be prepared could not be more urgent. The fact that that preparedness needs to involve telehealth to a large degree has become increasingly obvious. Sadly, due to the sluggish progress of regulatory, statutory, and legislative acceptance of the necessity and value this technology holds, we as a nation were not as prepared as other countries were. Those working on the federal and legislative levels are starting to do their part. So start preparing today! Find what method of telehealth integration works for your providers, patients, and workflow – and do it quickly. There is no time to waste when the health of not only a country, but an entire planet could rest on how swift and comprehensive our response is when this crisis hits its apex.
To learn how SimpleVisit can help you implement and utilize telehealth today, complete the telemedicine buyers guide or find out more about SimpleVisit’s managed telemedicine service.
5 Reasons Why Patients aren’t Using Your Telemedicine Program
Best Practices | August 14, 2019 In the healthcare industry, the benefits of telemedicine are widespread and commonly understood. Integrating video appointments into your practice is no longer considered revolutionary. If you are one of the many providers who have...
J.D. Power Telehealth Satisfaction Survey
Industry Update | August 5, 2019Early Results Give Insight into Lack of Patient Adoption Direct-to-patient telemedicine has grown beyond novelty to notoriety, warranting the attention of national consumer reports to generate a quality standard for this emerging...
ATA: State of the States 2019 Report
Industry Update | July 31, 2019The American Telemedicine Association (ATA) has recently released one of the most comprehensive surveys of legislation and reimbursement for telehealth services in the nation… and reveals an encouraging glimpse of the future. The ATA is...