
Reinvent Mental Healthcare: Think Like a Startup
STARTUP:
“A company working to solve a problem where the solution is not obvious and success is not guaranteed” – Neil Blumenthal, cofounder and co-CEO of Warby Parker.(1)
INNOVATE:
To make changes in something established, especially by introducing new methods, ideas, or products; to do something in a new way.
If we look at our current societal culture, we see that not only is it advanced, but it is advancing quickly. Many providers, truly the practice of healthcare in general, are behind the times, outdated, old, and antiquated. Medicine in practice needs to catch up, or we as a society will not be around much longer to realize the potential that our advancing technology has to offer. We will not be able to continue this great headlong rush down the hill of discovery and innovation much further because we will crash and burn if we cannot care for ourselves better. In the United States over the last 20 years, between 1997 and 2017, the death rate increased over 55%, with about 500,000 more deaths per year. In the world, almost 10 million more people died per year across the same span of time. (2, 3)
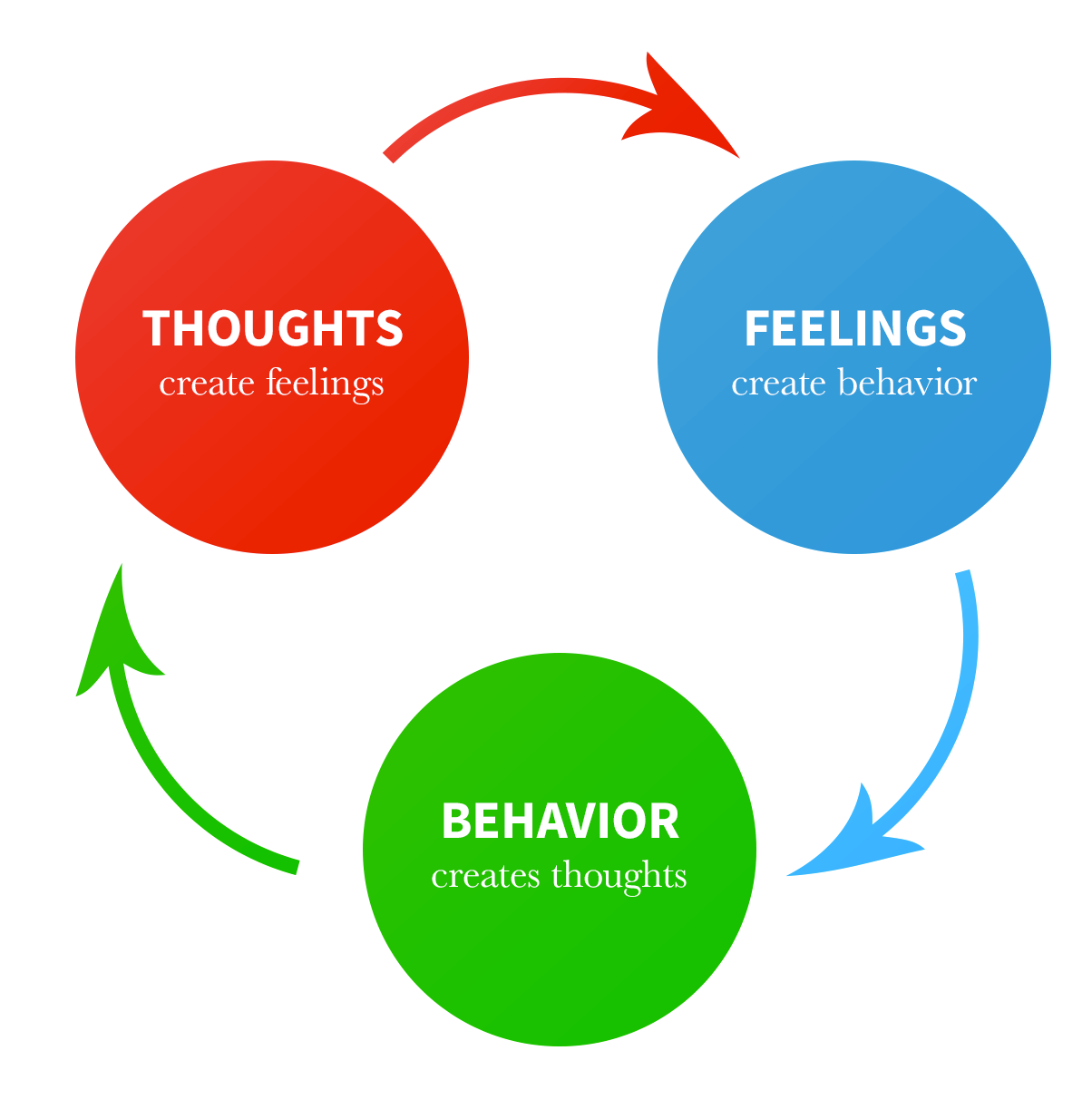
Addiction and substance abuse is a direct result of poor mental health processes, a disruption of what is known as the cognitive-behavioral triangle – and it is contributing to this rush towards cultural demise faster than most realize.
(Image: The Cognitive Behavioral Triangle)
According to the 2017 National Survey on Drug Use and Health:
- 3.2 million adolescents (age 12-17), 4.4 million young adults (age 18-25), 7.6 million adults aged 26 to 49, and 5.2 million adults aged 50 or older had a Major Depressive Episode (MDE) during the past year.
- That’s 20.4 million people with a Major Depressive Episode, along with another 29.4 million adults aged 18 or older with other kinds of mental illnesses.
Contrast that with this:
- In the entire population of age 12 or over, 48.7 million were current cigarette smokers, 140.6 million were current alcohol users, 30.5 million were currently using an illicit drug, and 19.7 million had a diagnosed substance use disorder (SUD) in the past year
Their analysis of documented statistics looks like this:
- 1.4 percent of all adolescents had an SUD and a Major Depressive Episode and 3.4 percent of all adults had both any mental illness (AMI) and at least one diagnosed SUD in the past year.
Lastly, there’s this:
- In 2017, 10.6 million adults aged 18 or older had thought seriously about trying to kill themselves (4.3 percent of adults), 3.2 million had made suicide plans (1.3 percent), and 1.4 million made nonfatal suicide attempts (0.6 percent).
- 47,173 Americans died by suicide, with an average of 129 suicides per day(4).
- And, since 2008, suicide has been #10 in the leading causes of death in the US.
In light of all of that, one can easily argue that the practice of treating Mental Health is THE SINGLE MOST IMPORTANT discipline. Studies show that your mental health, including your thoughts and feelings, effect EVERY OTHER mechanism in your body – there is a well-documented mind-body connect.
This is even more true of those who abuse illicit substances. In their article Drugs, Brains, and Behavior: The Science of Addiction, the National Institute on Drug Abuse states that, “People with addiction often have one or more associated health issues, which could include lung or heart disease, stroke, cancer, or mental health conditions.” Some of the health consequences of commonly abused drugs include:
- Marijuana: bronchitis, chronic cough,
- Cocaine: digestive problems, insomnia,
- Inhalants: muscle spasms and other permanent motor impairment, liver and kidney damage.
- Heroin: collapsed veins, abscesses, infection of heart lining and valves, arthritis, diseases transmitted through the blood such as HIV and Hepatitis C. (5)
But it is not only the drugs that affect your health negatively – just your overall state of mental well-being can affect your body in many ways. Physical health conditions improve in direct relation to how good or bad you think and feel – its causative, not correlative. Take a look at these statistics:
- People with the highest levels of self-rated distress (compared to lowest rates of distress) were 32% more likely to have died from cancer (6)
- Depression has been linked to a 50 percent increase in a person’s risk of dying from cancer and a 67 percent increase from heart disease. (7)
- In one study, researchers examined the association between “positive affect” — feelings like happiness, joy, contentment and enthusiasm — and the development of coronary heart disease over a decade. They found that for every one-point increase in positive affect on a five-point scale, the rate of heart disease dropped by 22 percent. (8)
- Adults with serious mental illness like schizophrenia are 3.4 times more likely to die of heart disease or diabetes, 3.8 times more likely to die in an accident, 5 times more likely to die of respiratory ailments, and 6.6 times more likely to die of pneumonia or flu.
But, there is hope:
- About 80 percent of people treated for depression with drugs and therapy improve, according to the National Institute of Mental Health. (9)
- Studies are constantly proving that there is measurable value and improvement in chronic illness and pain conditions using mental health strategies for stress reduction and psychological treatment. (10, 11)
So how do you, a passionate, dedicated mental health provider, do your part in keeping up with the times? How can you, who wants nothing more than to help the people of this world improve their minds so they can improve their bodies and lives so we can all keep improving our society and world, fully utilize the technology that is so readily available but so widely underused to help better your practice and your patients’ lives?
There is one word that encompasses the next frontier of medicine: telehealth. Evolving with new technologies and new ways to interpret virtual care, this innovative approach to medicine has been expanding and growing by leaps and bounds. We are learning how to apply what has already been invented to our current processes, and realizing what else needs to be invented so we can succeed in telehealth. We have stethoscopes that transmit data across bluetooth connections to a computer, pills that transmit live and continuous readings to wireless databases in the cloud, self-propelled carts delivering medication unmonitored by human hands. We have apps that can deduce when a person is in a life threatening situation and call for help for them by their own digital decision-making processes, and electronic surgical instruments that can be guided in real time by a robot controlled by someone with a joystick hundreds of miles away.
One can argue, though, that mental healthcare is the simplest and most unchanging discipline. We don’t need fancy tools to talk to someone, to listen to what they have to say, to give advice and guidance. We benefit from those tools as we gain a greater and greater understanding of the human brain and how it works and interacts with the rest of the body. There is a saying that we understand very little about life in outer space, we understand even less about life on the bottom of the ocean floor, and we understand even less about how our own brains do what they do. We discovered two new organs in the past year alone (interstitium and mesentery) in a field of study (medicine) that has existed since as early as 2000 BCE – that’s over 4000 years!
What mental health practitioners do at the core of that work is about connection. It’s about reaching people, seeing what’s going on in people’s lives, making them feel heard and validated and important, helping to empower and equip them to make better decisions, to change their feelings by changing their thoughts and actions, to improve their life and circumstances and what’s going on around them by processing and dealing with what’s going on inside of them. And the core of what telehealth is all about – using technology to bring your speciality of care to people who are not in the room, sitting beside your or in your immediate grasp – so seamlessly supports that process and purpose. It is a wonder it hasn’t had more traction until now. Why might that be? Is it because we’re scared of technology, or have a lack of understanding? Like teaching an old dog new tricks, you might think it’s impossible to go through more training to do something new in your field of business.
But it’s not new. All along, you’ve been practicing mental healthcare in the same way its been done since the deinstitutionalization movement of the 1950s – for almost 70 years. In your everyday life, you’ve been learning the technology at the core of telehealth in a shorter amount of time with ease. A basic timeline of the technology: computers only became available to the public in 1976, while cell phones became available in 1983. The network of information we call the World Wide Web was invented in 1990. Skype first started the video calling revolution in 2003, but there have been mentions of “videophones” in popular literature as early as in the cartoon “Edison’s Telephonoscope” by George du Maurier in Punch 1878. According to the Pew Research Center, “the vast majority of Americans – 95% – now own a cellphone of some kind. The share of Americans that own smartphones is now 77%” – all of which have embedded video-calling apps. That is all it takes to implement telehealth, especially in a field where most of your doctor-to-patient interaction is talking and listening. Only 43 years ago, this technology was unheard of, but today telemedicine is at our fingertips. Daily, we use the same technologies in our life that are used in virtual care, as simply as pushing an icon that looks almost exactly the same as the icon to make a regular call.
Think of how you could better care for your patients if you brought your practice of mental healthcare out from under the shadow of tradition and into the 21st century you’re living in.And what if all you needed to do that was push that little phone icon to answer a call? No downloading, no new applications, hardware, or software — just pick up the phone. If you did that, how many more people could you help? Think of the possibilities that would be presented if you were not limited by your or your prospective patients’ locations, by the time that travelling and clinical processes take up in your day, or by the staff needed to run a clinic or office. By filling all that time with just helping people, you could you feel more fulfilled and satisfied that you are doing your best to do the only thing you wanted to do when you started your first day of college: help people. How many providers are frustrated that so much of their time is taken up with the BUSINESS that goes into providing care, rather than actually providing the care? If you could remove all that extra stuff that goes into running a healthcare business and just help people with their health, would you?
The long and difficult process of opening your own office usually takes years of hard work, saving up, setting money aside, signing contracts, hiring employees, furnishing and renovating offices, all before helping that first person. But what if you flipped that process upside down and could start making money and helping people first, to make it possible to create a location where you could see them in person.
What if this took nothing more than a subscription, like the one you are paying to Amazon to give you a better way to shop, or Netflix to give you a better way to be entertained, or AT&T to give you a better way of communicating – a subscription to give you a better way of seeing your patients when they are not in the room with you? Wouldn’t that be worth it?
We are declaring that now is the time to pursue innovation! Make the choice today to do something different, so you can make what is most important better. It is time to embrace your fears of the new and unknown, and indulge your curiosity in how you can do things differently so you can do things better. Fight the status quo and turn your practice into a startup today. You don’t have to be a young good-looking business executive with outrageous ideas and wild proposals to have a startup. You don’t have to have a crazy new invention or create a word, term, or process nobody has heard of before to have a startup. All you need is a drive to meet a need, to fill a void, a burning mission with clarity of purpose, and the willingness to do what you’ve been doing a new way.
This is telehealth.
About Simple Visit
SimpleVisit is a video service which allows patients and providers to connect over the video platform of their choice. With SimpleVisit providers are able to deliver on-demand visits to patients over any device or platform they have available to them. For more information on SimpleVisit and on how we are enabling providers to host virtual visits check out www.SimpleVisit.com
How to Talk to Seniors (About Telemedicine)
Allie Clark | 10 min read | November 13, 2020In the midst of an unprecedented healthcare crisis, it’s important to be mindful of some of the most vulnerable members in our communities: our seniors. This particular season has been uniquely challenging for older...
The Journey Through
Allie Clark | 10 min read | October 28, 2020The lingering uncertainty of the pandemic in America is causing consumers and practitioners to adjust and re-adjust expectations for healthcare delivery. Regulators are changing their stance on privacy and coverage...
How to Launch a Successful Telemedicine Program
Rob Warlick | 5 min read | October 13, 2020Telemedicine has moved beyond intriguing to imperative in a short amount of time. Medical groups across the country are faced with the challenge to build and maintain a successful telemedicine program simply to retain their...



